
Part 1: How Can We Optimize the Health Workforce During COVID-19 and Beyond?
July 26, 2021 | 6 Minute ReadThe COVID-19 pandemic has accelerated the need for country leaders to optimize their existing health workforce to meet already high and now growing demand. But how can they do this? In a two-part series, we provide short- and long-term recommendations for health worker optimization within broader health system strengthening efforts.
Before COVID-19, health workers were already in short supply in many countries. The World Health Organization (WHO) identified 57 countries that have critical health workforce shortages, and it estimates a global health worker shortage of 18 million by 2030, primarily in low- and middle-income countries. Since the pandemic began, health workers have often been pulled from other services to respond to the emergency, challenging the health system to maintain the provision of essential services. As well, COVID-19 has degraded the global health workforce: Health workers have died from the disease or chosen to leave the profession; others succumbed to the physical and psychological toll. In short, they are overburdened, under-protected, stressed, and worn out. The pandemic has accelerated the need for country leaders to optimize their current health workforce to meet high and growing demands. But how can they do so?
Through USAID’s flagship global health workforce program, Human Resources for Health in 2030 (HRH2030) — led by Chemonics, with consortium partners the American International Health Alliance (AIHA), Amref Health Africa, Open Development, Palladium, ThinkWell, and the University Research Company (URC) — we have worked over the past six years to support, optimize, and invest in the health workforce in more than 30 low- and middle-income countries.
In this two-part series, we call for country leaders to consider whether they are sufficiently optimizing their health workforce to respond to the pandemic and to contribute to longer-term health system resilience. We offer resources and tools to help leaders ensure uninterrupted care and continued provision of high-quality health services. We provide six key recommendations split between the two parts: In Part 1 we consider the following short-term approaches— 1) employ and expand task sharing, 2) professionalize and fully engage community health workers (CHWs), and 3) expand digital health learning and mobile applications; and in Part 2 we share approaches for sustainable investment to optimize the health workforce and strengthen the health system in the longer term.
Part 1: Three Short-Term Recommendations
1. Employ and expand task sharing to increase access to services

When hiring more health workers to fill gaps is not an option in the short term, increasing the performance and productivity of existing health workers is imperative. Task sharing helps health leaders to redistribute responsibilities from higher-skilled health workers to those with less training, expanding the number and types of health workers who can provide services. Task sharing frees the health workers with advanced clinical skills to provide services to clients who have critical health needs or complicated diagnoses and treatment plans. For example, task sharing can increase clients’ access to services when some tasks that were previously performed by only physicians may be performed by nurses, as well. Tasks that were performed by nurses or midwives may be done by CHWs, safely and effectively bringing services to the community and the individuals who need them.
In family planning, for instance, nurses, midwives, and assistant midwives who have undergone competency-based training can safely insert and remove contraceptive implants — something previously done only by doctors — and well-trained and monitored CHWs can safely provide contraceptive injections and offer education, counseling, and other short-term contraceptive methods — tasks previously handled only by nurses and midwives. This task sharing can help maintain the continuity of services to achieve global family planning goals.
As countries have begun to adopt task-sharing policies, HRH2030 research, led by Palladium, examined national family planning guidelines in 10 countries to consider how well they adopted policies or service delivery guidelines in line with WHO guidelines on task sharing and self-care. The HRH Optimization Tool for Family Planning (HOT4FP, available in English and French), developed with partner URC, can be used to promote client-centered services through task sharing and adapting service delivery models to expand service provision beyond facility walls.
2. Professionalize and fully engage CHWs to expand health system reach

Community health approaches — and well-trained, managed, and motivated CHWs — are vital to the delivery of primary health care services. By contributing to population health outcomes, CHWs strengthen health systems and move us closer to achieving health for all to reach global health goals.
In October 2018, the WHO released the “guideline on health policy and system support to optimize community health worker programs” with 15 important recommendations for professionalizing CHWs, properly integrating them into health systems and communities. To build on these recommendations, HRH2030 supported the development of the USAID Flagship CHW Resource Package, an online platform for tools, research, guides, and best practices that strengthen CHW programs. Resources for maximizing the existing workforce include a toolkit, Optimizing Health Workforce Performance and Productivity to Achieve the 95-95-95 Targets.
While these suggestions focus on fully engaging the existing community health workforce, health workforce decision-makers also need to plan for the future. Through partner Thinkwell, HRH2030 created a new econometric forecasting model, the Comprehensive HRH Assessment, Modeling, and Planning Solution (CHAMPS). By exploring the forces that influence health worker supply and demand — changing economics, disease burdens, and population shifts — CHAMPS enables HRH planners to calculate country-specific health worker projections and prepare for health labor market changes. This effective forecasting allows the efficient allocation of scarce resources, including finances, to ensure CHW integration and remuneration.
3. Expand digital health learning and mobile applications to improve health workforce preparedness and resilience
Continuous professional development is important for health workers to stay current with the latest research and technologies, emerging health issues, new treatment programs, and licensing requirements. Training health professionals through online learning platforms and apps is not new, but it has proliferated during the pandemic. A well-trained, well-supervised, and well-resourced health workforce is not only essential to emergency preparedness, but also to achieving health for all. HRH2030 has undertaken several initiatives that demonstrate the value of online and mobile health workforce training. For instance, in the Philippines, HRH2030 worked with the Department of Health through AIHA to launch an e-learning platform, the DOH Academy. During the past year, the DOH has created an entire menu for health worker training, including modules on COVID-19. It has proved to be a supremely efficient way for health workers to access learning modules anytime, anywhere, saving travel time and enabling them to spend more time providing direct patient care. When COVID-19-related travel restrictions were in place, accessibility to online learning meant that health workers could continue to access critical learning, without risking infection or spreading disease in a classroom or facility.
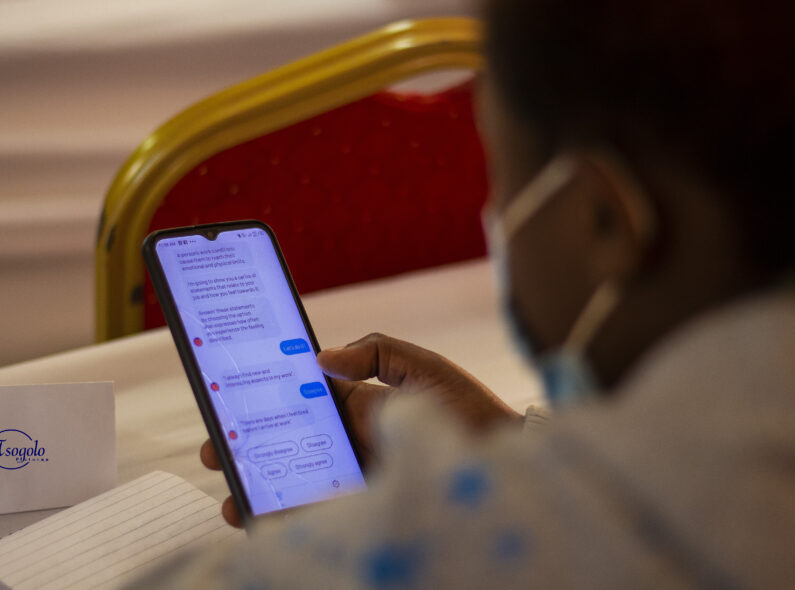
Other digital health innovations have been designed and scaled during COVID-19, including mobile health apps and technologies that support contact tracing, surveillance, diagnostics, and clinical decision support, among others. Mobile technology is now being used to support the mental health and resilience of health workers, which has proved to be particularly important during the current health emergency.
For example, the mental health chatbot Vitalk is a mobile app that can screen health workers for anxiety, burnout, and depression. It provides psychosocial support to address specific challenges that health workers are dealing with during COVID-19; it also refers those who need additional resources to a human service provider. Piloted in Brazil with 5,000 workers, mostly nurses, initial research shows that the digital tool is having an impact, with 85 percent of users describing the experience as positive or very positive. HRH2030 is working with Vitalk-developers to adapt the digital innovation to use in sub-Saharan Africa.
***
As we have learned from the COVID-19 pandemic, health system changes can be made quickly when there is commitment and understanding of their imperative, especially during an emergency. Now is the time to safeguard, protect, and invest in health workers around the world to meet current and future health care needs. In the short term, we call for countries to examine whether they are fully optimizing their existing health workforce and, if not, to 1) employ and expand task sharing to alleviate workloads and meet critical health needs; 2) professionalize and fully engage CHWs, with their immeasurable value in expanding primary health care service delivery; and 3) expand digital health learning and mobile applications to provide accessible, affordable capacity building, health care provision, and mental health support for health workers.
Read the next installment of this series, “Part 2: How Can We Optimize the Health Workforce in COVID-19 and Beyond?” with three long-term recommendations for health worker optimization. Learn more about HRH2030’s impact through its series of legacy events.
Banner image caption: Dr. Wilson Ching’ani (third from left) and his team stand in front of Zomba District Health Office in Malawi. Credit: HRH2030.
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.


































