Enhancing Pharmaceutical Supply Chain Management for Improved Health Outcomes
June 23, 2022 | 4 Minute ReadThe development of strategies for optimal pharmaceutical supply chain management is important to establish secure and efficient procurement and delivery procedures for essential medicines, in the pharmaceutical sector for low-to-middle-income countries (LMICs).
The World Health Organization (WHO) estimates that approximately two billion people around the world do not have access to necessary medicines, vaccines, medical devices, and other health commodities. In addition to the limited access to medicines, 10.5% of all available health commodities are classified as substandard or falsified, which harm patients, healthcare economies, and supply chains. Efficient pharmaceutical systems that regulate, supply, and promote the appropriate use of essential medicines and other health commodities are key to meeting the health needs of a population. Achieving this in lower- and middle-income countries (LMICs) requires streamlined coordination between many stakeholders, including manufacturers and distributors, government bodies serving as regulators and policymakers, healthcare providers such as public and private hospitals, non-profit organizations, pharmacies and community health workers, donors, among others. Each of these organizations has different objectives, which adds to the complexity of having an efficient and effective pharmaceutical system.
While some LMICs have established secure and efficient procedures to ensure the quality of essential medicines, many of them lack a comprehensive pharmaceutical system that includes strong governance, effective regulations and enforcement practices, appropriate financing and capacity, and reliable product and patient or end user information that ensure the quality, safety, and efficacy of medical products. To address these challenges, countries need to strengthen health systems as a whole to help detect, assess, and mitigate adverse events, medicine use errors, and therapeutic failures.
Below we describe illustrative challenges of pharmaceutical supply chains in LMICs and how strengthening pharmacovigilance capacity and improving service delivery through pharmacy services promotes pharmacovigilance within the health supply chain.
Establishing and Strengthening Pharmacovigilance Capacity the Supply Chain
One major challenge pharmaceutical supply chains in LMICs face is the maintenance of quality drugs after they have been licensed for use, also known as pharmacovigilance. Pharmacovigilance is the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or problems relating to medicine. A majority of LMICs are classified as having minimal or basic pharmacovigilance systems to guarantee reporting of adverse drug events by healthcare workers. Because drug-related harm includes adverse events or reactions, medication error or side effects, and harm that may not have occurred during the drug development stage, it is pertinent that more focus is placed on developing systems for drug safety monitoring. Implementation of such systems requires all stakeholders working in the supply chain to have a patient-centered approach that ensures patients have access to medicine products proven to be safe and efficacious within a timely manner.
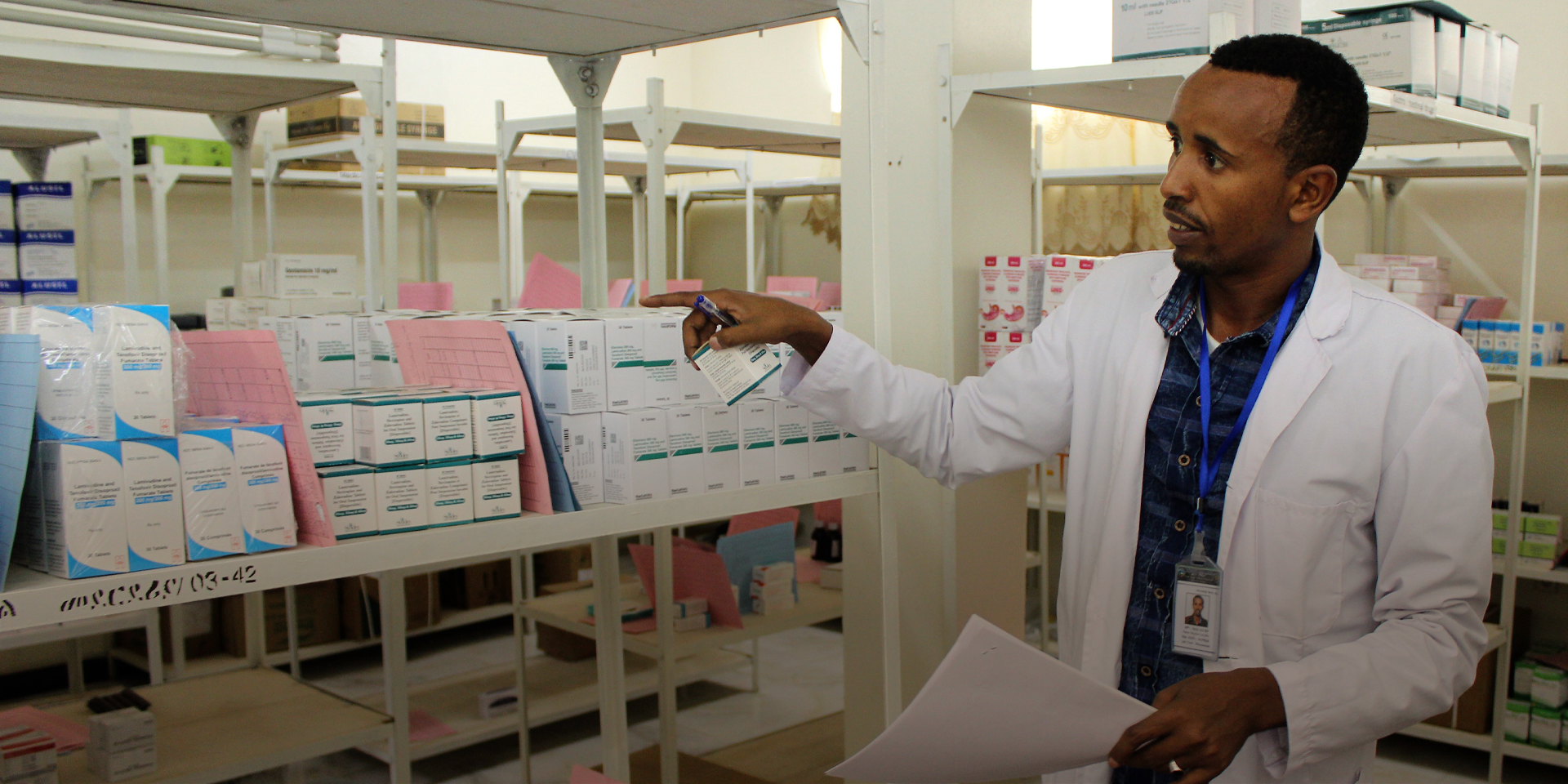
Our Global Health Supply Chain program – Procurement and Supply Chain Management project’s (GHSC-PSM) has been working with the Ethiopia Food and Drug Administration (EFDA), regional health bureaus (RHBs), and regional health facilities on strengthening national efforts in monitoring, preventing, detecting, and reporting adverse drug effects (ADEs) from antiretroviral drugs used in HIV therapy, anti-TB drugs, and other medicines. Because of the central role healthcare workers have in patient safety, GHSC-PSM and EFDA designed and developed a national pharmacovigilance training course aimed at improving knowledge, attitudes, and practice of healthcare providers in the detection, prevention, and reporting of ADEs. Within two years, reporting of ADEs increased two-fold and health facilities have a self-sustaining and reliable pharmacovigilance system to operate with. GHSC-PSM continues to support and work collaboratively with stakeholders in building capacity in the Ministry of Health (MoH) health programs to strengthen drug safety surveillance activities in Ethiopia.
Improving Service Delivery Through Strengthening Pharmacy Services
The quality of pharmaceutical services varies across countries, and many LMICs have reported on the inadequacies of pharmacy practices such as issues relating to dispensing activities, labeling, information about medicines and their usage, and advice to patients or end users. Additionally, often there is not a qualified pharmacist, or other suitably qualified staff, present to provide the needed services. Evidence in literature indicate that access to private pharmacies helps with overcoming barriers to access due to more convenient geographic location, provide extended hours for patients, and a private environment for those who may fear stigmatization due to their conditions.
Our GHSC-PSM in Mozambique has supported the successful implementation of Decentralized Drug Distribution (DDD PP) for anti-retroviral (ARVs) through private pharmacies in partnership with MoH, PEPFAR, the USAID funded EPIC project implemented by FHI 360, and other implementing partners. The program consisted of the establishment of a MoH-led governance structure to promote transparency and accountability, training of pharmacy staff, and the potential to increase patient adherence with the use of a tracking system known as iDART. The program has resulted in 72 pharmacies dispensing ARVs with patient referrals coming from 39 public health facilities. Additionally, over 17,000 client enrollments have been reported and increased access to critical medicines during weekend hours has been provided to 8.4% of enrolled clients. Based on the current success of the DDD PP program in Mozambique, there is potential for expanding services to other disease areas such as pre-exposure treatment of HIV, the inclusion of additional health facilities and private pharmacies, and an expansion of services offered to patients during their pick-ups. This is an approach that can be replicated in other countries for the benefit of the global health supply chain.
Despite the challenges in access to and proper regulation of pharmaceuticals in LMICs, strengthening pharmacovigilance capacity as well as pharmacy services serve as key examples of patient-centered approaches to strengthen pharmaceutical systems that provide reliable access to quality health care services to the populations we serve.
Banner photo caption: Pharmacist handling ARV medication in Pharmacy in Ethiopia, GHSC-PSM Ethiopia
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.