3 Questions with Kesaobaka Dikgole: Delivering Differently for HIV Clients in Botswana
August 21, 2018 | 4 Minute ReadWith high caseloads and a limited number of healthcare staff, countries like Botswana need innovative ways to bring HIV care services closer to where people live and work. Kesaobaka Dikgole discusses the role of differentiated care models in strengthening the health system.
This post originally appeared on the HRH2030 blog.
Kesaobaka Dikgole is a senior quality improvement advisor with HRH2030 in Botswana while also serving as a country representative for the University Research Co. (URC). She oversees the technical team to design, test, and evaluate care innovations to improve patient-centered HIV care as part of PEPFAR efforts to control the AIDS epidemic in Botswana.
What are the greatest challenges related to the health workforce in Botswana, particularly as they relate to HIV service delivery?
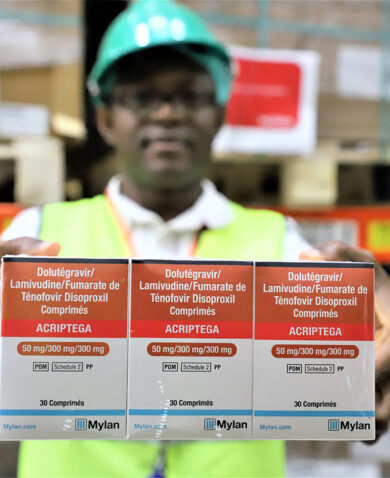
Botswana remains one of the countries most affected by HIV/AIDS. Fortunately, not many people are dying due to AIDS these days, but close to one in four Batswana need regular, reliable access to the medical system — for life-saving drugs and routine check-ups — for the rest of his or her life.
The greatest challenge from a human resource perspective is the high caseload itself, including many clinically stable clients who come to facilities for monthly drug refills. Managing this traffic puts a huge burden on already strained staff, especially as some types of health workers are scarce and unevenly distributed across the country. A related challenge is that HIV care is often delivered through a stand-alone, facility-based program instead of being integrated with other primary health care services. This is challenging for clients who need care for other conditions, in addition to HIV, or who want to bring along their children or other relatives for care at the same time. Unfortunately, they need to get separate appointments and make multiple visits.
While it was the success of these vertical efforts that allowed Botswana to prevent AIDS-related deaths, it has come at a high cost for the system as a whole. Today, many health workers express their frustrations serving in a fragmented and disjointed system and their conviction that the time has come to re-integrate under a holistic approach to primary health care. They see this as a necessity for their own and their clients’ sake and for that of the system’s long-term sustainability. This is why HRH2030 in Botswana is supporting efforts by the Ministry of Health to make basic, integrated HIV services available within the community itself, including support for new models of care that bring services closer to where people live and work.
Botswana’s Ministry of Health and Wellness, PEPFAR, and other stakeholders agree that changes are needed in the way HIV services are provided and delivered within and outside of facilities. How does differentiated care promise to improve quality of HIV care in Botswana?
Botswana has come a long way — from seeing its people’s life expectancy plummet by 20 years due to the sudden explosion of AIDS-related deaths to nearing achievement of epidemic control. But even with that success (and because of it), the number of Batswana who live with the virus and depend on life-long treatment keeps increasing. While generally reflecting progress, this trend increases the burden on an increasingly fragile health system, which is also a victim of the epidemic.
The Government of Botswana has recognized this challenge and declared its determination to “transform health” through the revitalization of primary healthcare. At the core, the Ministry of Health and Wellness has identified the need to bring health services closer to communities, strengthening their involvement in all health matters. This includes not only a greater emphasis on personal responsibility for wellness and healthy lifestyles but also a systematic rethinking of how the system is delivering services to those who need them.
Differentiated care, an approach to how services are delivered according to the needs and expectations of clients, has established itself as a pragmatic way of making progress. Practical examples in Botswana focus on encouraging district health management teams to partner with NGO health care providers in their districts to “deliver differently.” This means that care provided to newly diagnosed clients looks different from care provided to those who are stable and on treatment or to clients who need care for more than one chronic condition. The goal of our focus on differentiated service delivery is to improve client care, in very practical ways, by re-organizing around their needs. At the same time, we can address acute systemic bottlenecks and burdens on health workers and support functions within the communities. In Botswana, HRH2030’s support of this win-win approach is unifying partners around one agenda.
How is HRH2030 supporting the adoption and scale-up of differentiated care models in Botswana?
Due to Botswana’s massive and prolonged emergency effort to identify people living with HIV, to initiate their treatment, and to keep them on treatment, health care provision in Botswana has become increasingly medicalized and fragmented. In contrast to Botswana’s traditional approach of community-based primary health care, services today are largely provided by facilities waiting for sick clients to come to them for curative, rather than preventive services.
Adapting the system’s existing models of disease-focused care for HIV, tuberculosis, diabetes, cancer, or hypertension, to become more integrated and holistic will have important implications for the health system, including the organization, training, and allocation of health workers. How human resources for health are deployed and supported needs to be at the center of any effort to transform and improve health systems.
HRH2030, in partnership with USAID through PEPFAR, is working very closely with Botswana’s Ministry of Health and Wellness at the central, district, and community levels to analyze, understand, and adapt existing models of care to make them more client-centric, integrated, and efficient. We follow a collaborative, step-by-step approach that applies systematic quality improvement methods — coaching dedicated health services delivery improvement teams to analyze problems and barriers, develop change ideas, test these changes to improve care, and evaluate improvement efforts. At the request of the ministry, we are currently collaborating with the Greater Gaborone District Health Management Team and its partners, including USAID’s Advancing Partners & Communities project, to adapt service delivery in a phased manner beginning with the Old Naledi community in Gaborone. By following a collaborative improvement approach to differentiate service delivery, we can improve the quality of care, use scarce resources efficiently, and reduce the burden on the health workforce.
Blog posts on the Chemonics blog represent the views of the authors and do not necessarily represent the views of Chemonics.